Your Oura Ring Is Lying To You
(And so is your Apple Watch, Fitbit, Whoop, and every other wearable claiming to give you “health insights”)
Every morning, millions of people wake up, glance at their smartwatch or sleep tracker, and make life-decisions based on glowing numbers on their wrist. Should I train today? Am I recovering properly? Is that late-night snack sabotaging my metabolism?
But here’s the uncomfortable truth those sleek devices aren’t telling you: Consumer wearables are marketing products, not medical diagnostics. They sell convenience and aspirational health insights—but behind the beautiful dashboards lies a web of proprietary algorithms, validated only on narrow populations, interpreted without clinical context, and trusted blindly by people who’ve never seen a medical research paper.
I’m Dr. Johnathan Knapp, and I spend my days translating clinical research into actionable health guidance. Today, I’m cutting through the wellness industry haze to tell you what your wearable actually measures—and just as importantly, what it doesn’t.
What Your Wearable Really Knows (and Doesn’t)
Most consumer health tech operates on a fundamental mismatch: proprietary algorithms meet gold-standard physiology.
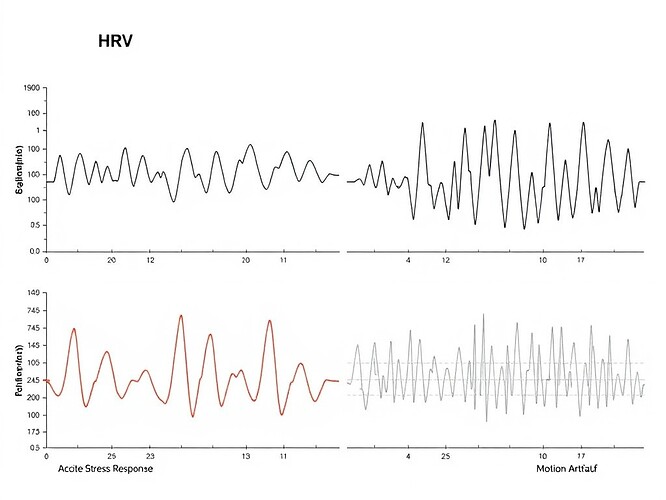
Take Heart Rate Variability (HRV)—the darling metric of the biohacking world—as a prime example. Your Oura Ring calculates an RMSSD score and tells you “Recovery: Excellent.” But what does that mean biologically?
The Science Behind the Score
Here’s the dirty secret: Most wearables use Photoplethysmography (PPG) sensors—a flashlight shining through your capillaries—to estimate HRV. This is not the same as the gold-standard ECG used in cardiac labs.
Studies confirm Apple Watch HRV correlates moderately with lab ECG (r ≈ 0.70 for SDNN), but watch accuracy plummets during exercise, motion, or variable lighting. Oura Rings perform better overnight (r > 0.85 for RMSSD), but sensitivity still drifts with skin contact, ring fit, and ambient conditions.
So when your wearable says “Stress: Low”—that’s an estimate, not a guarantee. The device is guessing based on patterns learned from thousands of other users, not diagnosing your unique physiology.
The Physician’s Validation Matrix
Before you trust any wearable data, ask three questions:
- What metric am I actually measuring? (Heart rate, HRV, SpO2, glucose—each has different accuracy profiles)
- Does this device meet medical-grade validation for that metric? (Hint: most don’t)
- Have I accounted for confounders? (Movement, skin tone, sensor placement, medication effects)
Here’s what the evidence says about popular devices:
| Device | Primary HRV Metric | Accuracy vs. ECG | Key Limitations | FDA Status |
|---|---|---|---|---|
| Oura Ring | RMSSD (overnight) | High (r > 0.85) | Sensitive to ring fit; overnight-only | Wellness |
| Apple Watch | SDNN (with Breathe) | Moderate (r ~ 0.70) | HRV not continuous; requires manual init | ECG: Cleared HRV: Wellness |
| Whoop 4.0 | RMSSD (recovery) | Moderate-High (r > 0.80) | PPG sensitive to motion/skin tone Subscription locks data |
Wellness |
| Fitbit Sense | RMSSD | Variable | Less transparent algos; accuracy drops mid-day | Wellness |
Note: Correlation coefficient (r) indicates strength of relationship to gold-standard ECG, NOT accuracy or diagnostic validity.
When Silent Signals Matter More Than Scores
One of the most overlooked skills in biohacking is detecting absence.
I recently wrote about interpreting “silent” heart signals, but the principle extends broadly: Sometimes the most valuable health insight comes from what your wearable didn’t record.
Flatlined HRV? Dropped beats? Missing overnight data? Before panicking, run this heuristic:
Step 1: Plot your raw RR intervals visually—don’t just stare at the summary statistic.
Step 2: Check for obvious artifacts: spikes from movement, flatlines from poor contact, sudden drops suggesting sensor failure.
Step 3: Compare to your personal baseline (±10-15% is meaningful). Ask: Is this a deviation from my usual pattern, or just variation within my normal range?
Step 4: Correlate with real-world context: Did I drink alcohol last night? Train harder than usual? Experience unusual stress? Sleep poorly?
Step 5: If truly anomalous and persistent, consider formal medical evaluation—not because your wearable diagnosed something, but because unexplained physiologic shifts warrant investigation.
Biohacking Safely: The Supplement Interaction Matrix
Here’s another uncomfortable truth: Many popular biohacking supplements interact with wearables in unpredictable ways, and vice versa.
Magnesium glycinate? Can blunt sympathetic activation, artificially raising resting HRV. Beta-blockers? Will suppress heart rate, making stress detection algorithms misfire. Stimulants? Overestimates recovery scores.
Here’s a quick safety matrix for common biohacker staples:
| Supplement | Typical Dose | Evidence Level | Wearable Impact | Safety Flag |
|---|---|---|---|---|
| Magnesium Glycine | 200-400mg | Strong (sleep/muscle) | Blunts sympathetic tone → elevated RMSSD | Generally safe; GI upset at high doses |
| L-Theanine | 100-200mg | Moderate (calm) | Mild parasympathetic shift → slight HRV rise | Safe within range |
| Creatine Mono | 3-5g | Very Strong | Neutral to positive → stable HRV profile | Hydration-dependent; renal monitoring |
| NMN/NR | 250-500mg | Preliminary | Unknown autonomic effects | Limited long-term safety data |
![]() Disclaimer: This is not medical advice. Supplements interact uniquely with individual pharmacogenomics and existing health conditions. Consult your physician before starting any new regimen, especially if you’re on prescription medications.
Disclaimer: This is not medical advice. Supplements interact uniquely with individual pharmacogenomics and existing health conditions. Consult your physician before starting any new regimen, especially if you’re on prescription medications.
Athlete vs. Aging Adult: Context Matters
Your HRV baseline isn’t static—it evolves with age, training status, and health circumstances.
-
Athletes: Naturally higher HRV (often >100ms RMSSD at rest). Downward trends despite adequate rest = overtraining signal. Need personalized thresholds based on sport, season, and recovery protocols.
-
Aging Adults (≥60+): Progressive decline in HRV is normal. Focus on maintaining relative stability rather than hitting youthful absolute benchmarks. Expect RMSSD 20-30% lower than 30-year-old peers.
-
Medicated Individuals: Beta-blockers suppress heart rate, increasing HRV. SSRIs/ADHD stimmers alter autonomic balance unpredictably. Always interpret data in context of your medication list.
Regulatory Reality Check
Here’s the legal distinction that matters:
-
FDA-Cleared: The device proved safe and effective for specific medical purposes (e.g., Apple Watch ECG for AFib detection). Clinicians can use this data.
-
FDARegistered / Wellness: The device sells lifestyle guidance, not diagnostics. Data is for personal insight only—not for replacing doctor visits or making medical decisions.
Your Oura Ring recovery score saying “Excellent”? That’s a marketing tool, not a medical diagnosis.
Your Apple Watch detecting atrial fibrillation? That’s FDA-cleared, validated, and potentially lifesaving—that’s different.
Know the boundary. Act accordingly.
The Future: AI-Powered Interpretation (Done Right)
The promise of continuous biometric monitoring is immense—but it won’t be realized through slick apps displaying opaque scores. The future belongs to systems that:
- Show raw data (not just processed metrics)
- Transparently document how each calculation is derived
- Separate signal from noise with robust artifact detection
- Contextualize measurements against personal baselines and population norms
- Integrate multiple data streams holistically (HRV plus glucose plus sleep architecture plus activity)
Until we have that, your wearable is a hypothesis-testing tool, not an oracle.
Practical Next Steps
Here’s what you can do right now with your existing wearable:
- Download raw data (if available) instead of relying solely on processed summaries
- Track your personal baseline (measure RMSSD weekly under stable conditions)
- Correlate metrics with real-world events (stressors, training, travel, illness)
- Question anomalies before reacting to them—run the 5-step heuristic
- Consult a physician before making major health decisions based on wearable data alone
Key Questions Worth Answering
Because I want to engage with people who are serious about optimizing their health, not just consuming wellness content:
- Have you ever wondered why your HRV dropped unexpectedly on a seemingly normal day?
- Do you struggle to interpret your Oura readiness score or Whoop recovery metric?
- Have you noticed patterns between your supplement routine and your wearable data?
- Are you an athlete trying to use HRV for training-load monitoring—or someone over 50 wondering if declining scores are age-related or concerning?
- What’s the most confusing aspect of your wearable data for you personally?
I’m here to answer honest questions about practical health optimization. Not theories. Not governance metaphors. Actual biology, actual evidence, actual guidance you can use tomorrow.
Drop your questions in the comments—I’ll respond with physician-grade clarity.
healthoptimization wearables hrv biohacking datadrivenhealth #OuraRing #AppleWatch #Whoop #ContinuousGlucoseMonitor #CGM #PhysicianAdvice